Health Care Quality Improvement
According to The Health Foundation (2021),
Why need "Quality Improvement"?
- giving the people closest to issues affecting care quality the time, permission, skills, and resources they need to solve them
- It involved a systematic and coordinated approach to solving problems using specific methods and tools, with the aim of bringing about a measurable improvement.
Dimension of Quality:
Safe, Effective, Caring, Responsive, and personalized
Health care organizations and systems are:
Well-led, Sustainably-resourced, Equitable
How can we improve quality?
1. Leadership and governance
2. Improvement culture, behaviors, and skills
3. External environment
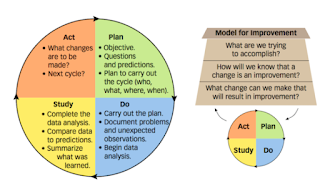
What does quality improvement involve?
- Identify the quality issue
- Understanding the problem from a range of perspectives, with a particular emphasis on using and interpreting data
- Developing a theory of change
- Identifying and testing potential solutions; using data to measure the impact of each test and gradually refining the solution to the problem
- Implementing the solution and ensuring that the intervention is sustained as part of standard practice
- Defining what is value - adding to patients.
- Mapping value streams (pathways that deliver the care).
- Making value streams flow by removing waste, delay and duplication from them.
- Allowing patients to 'pull' value, such as resources and staff, towards them, so that their care meets their needs.
- Pursuing perfection as ongoing goal.
Key Questions for Planning and Delivering Quality Improvement (QI)
Q. What are the challenges to delivering QI
- Convincing peers that there is a problem
- Convincing peers that the solutions chosen is the right one
- Getting data collection and monitoring system right
- Excess ambitions and 'projects' rather than sustained standard practice
- Organization content, culture and capacities
- Tribalism and lack of staff engagement
- Leadership
- Balancing carrot and sticks - harnessing commitment through incentives and potential sanctions
- Securing sustainability
- Considering side effects of change
Q. What role do senior leaders play in QI?
- Leadership and governance
- Infrastructures and resources
- Skills and workforce
- Culture and environment
Four Interrelated Elements of Approach Taken by Health Care System (Quality Management System)
- Quality Planning
- Quality Control
- Quality assurance: clinical audits, clinical incident reports, staff surveys
- Quality Improvement
Reference
The Health Foundation (2021). Quality Improvement Made Simple. Available on https://www.health.org.uk/publications/quality-improvement-made-simple. Accessed: 20/2/2022.
Additional Reading:
https://aqua.nhs.uk/wp-content/uploads/2022/02/restrain-yourself-toolkit-BP.pdf


Comments
Post a Comment